TAP THE ICON to learn more about the type of infection
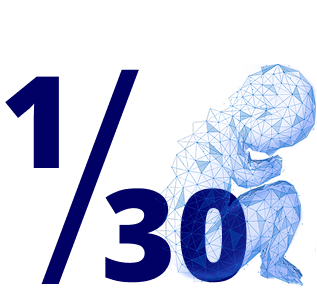
SEPSIS
(presence of bacteria in the bloodstream)
A life-threatening condition
Symptoms:
- Fever
- Chills
- Confusion or altered mental status
Complications:
- Limb amputation
- 1 in 30 children with pneumococcal sepsis dies from the infection
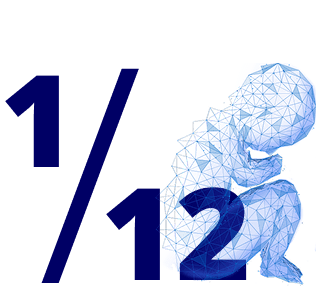
MENINGITIS
(infection of the membranes surrounding the brain and spinal cord)
Symptoms:
- Stiff neck
- Fever and headache
- Sensitivity to light
- Confusion or altered consciousness
- Vomiting, poor appetite
- Fatigue
Complications:
- 1 in 12 children with pneumococcal meningitis dies from the infection
- High risk of neurological impairment or hearing loss after recovery
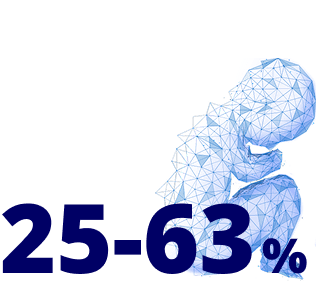
INVASIVE PNEUMONIA
(lung infection with bacteria present in the blood)
Symptoms:
- Fever
- Cough
- Shortness of breath
- Productive sputum
- Pleuritic chest pain
Complications:
- 30-day mortality is significantly higher in patients with bacteremic pneumonia (28.6%) compared to non-bacteremic cases (8.5%)
- Infection-related mortality is also higher in bacteremic pneumonia (19.5%) vs. non-bacteremic (4%)
ECONOMIC BURDEN

due to pneumococcal pneumonia occur each year in the United States.9
was spent annually on the treatment of community-acquired pneumonia in the U.S. between 1996 and 1998.10
higher: The healthcare costs for high-risk individuals with pneumonia compared to healthy individuals.11
Your may be at increased risk

You may be in a higher-risk group.

Worth your attention.Pneumococcus can lead to life-threatening diseases


What is Invasive Pneumococcal Disease?
Invasive Pneumococcal Disease is a dangerous infection caused by pneumococcus invading sterile areas of the body such as blood or the central nervous system. Invasive Pneumococcal Disease includes meningitis, bacteremia, and invasive pneumonia. 2
How is pneumococcal disease transmitted?
Pneumococcal disease spreads through direct contact with respiratory secretions, such as saliva or mucus. Children who are not vaccinated are at higher risk of infection, partly because their immune systems are not yet fully developed. 2
What are pneumococcal serotypes?
Serotypes are classified based on different structures on the surface of pneumococcus. Different serotypes of pneumococcus can cause a range of infections from mild to severe, depending on the characteristics of each strain. 3
How common is pneumococcus?
Nearly 60% of children have pneumococcus residing in the nose and throat. Pneumococcus is then transmitted to others via droplets and contact. 1
Can pneumococcus be actively prevented in young children?
Yes, contact your doctor for preventive measures.
How does pneumococcal disease affect children?
Severe cases of pneumococcal disease can cause death, neurological complications, hearing loss, delayed development, or limb loss.6